
Gonarthrosis is a pathological process in the cartilage tissue of the knee joint, which leads to deformity of the knee joint. This process is associated with high stress in the knee, wear and salt deposition.
Myths about gonarthrosis
There are 3 most famous myths:
- "Diagnosing gonarthrosis is the prerogative of people who are physically active, and people who are primarily sedentary do not suffer from it. "In fact, overexertion actually contributes to the decline. cartilage degeneration. During sedentary work, static electricity occurs to the knee, the blood supply is obstructed. In addition, a sedentary lifestyle leads to an increase in body weight.
- "Knee warts cannot be cured, the disease is progressing day by day". This disease is truly chronic, but with adequate timely treatment, cartilage deterioration can be prevented.
- "With akylosing spondylitis, you need to move as little as possible and lie down more. "A patient with such a pathology is assigned special gymnastics, which strengthen the ligamentous apparatus. Only certain sports are really contraindicated.
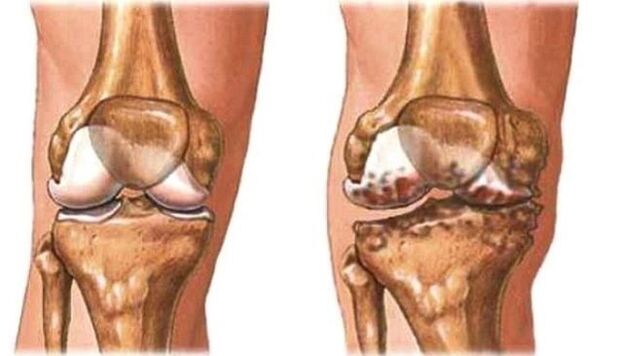
Gonarthrosis is the destruction of articular cartilage in the knee joint and adjacent bony surfaces.
Manifestations of knee osteoarthritis
Manifestations depend on the severity of the malformation. The more pronounced, the more pronounced the symptoms.
Symptoms of Gonarthrosis:
- long periods of no symptoms;
- discomfort in the knee area;
- pain syndrome;
- reduced mobility;
- morning stiffness up to half an hour;
- the presence of a crunching sound during active movement;
- change in gait.
Bilateral gonadalitis occurs when the knee joints of both extremities are involved in this process. This is one of the most severe forms. Occurs in the elderly.
Right-sided gonarthrosis occurs with excessive static or dynamic exertion in the right extremity. More often in athletes.
Left-sided gonarthrosis occurs in overweight individuals and in athletes with a load on the left leg.

The reasons for the development of gonarthrosis
Gonarthrosis is primary and secondary. Primary can occur in childhood and adolescence, is associated with joint deformities, as well as in the elderly due to the natural aging process.
Secondary occurs due to trauma or existing diseases. Main reason:
- fractures, bruises, dislocations;
- excess weight;
- the presence of inflammatory processes in the joints and the lack of appropriate therapeutic therapy;
- metabolic diseases, which are accompanied by the deposition of salts in the cartilage tissues;
- activities;
- Vitamin D deficiency;
- Hormonal disorder;
- lift the weight;
- some sports (running, hockey, football).
Who is at risk?
The risk group includes:
- professional athletes;
- obese people;
- the patient has undergone trauma or surgery;
- people over 45 years old;
- patients with varicose veins;
- who have had arthritis in the family.
The risk group also includes women who wear high heels or flat soles.

The exact cause of knee effusion is still unknown.
Degree of gonarthrosis
Radiologically, this pathology is divided into 5 stages or degrees:
- Stage 0 - X-ray without joints;
- Stage 1 - the appearance of a small bone cell;
- Stage 2 - bone mass with clear contours, minimally altered joint space;
- Stage 3 - narrowing of joint space;
- Stage 4 - marked narrowing of the space, hardening of the subchondral bone.
Knee gonadal inflammation 1 degree
The first degree is characterized by fatigue, mildly limited movement, and audible crunching. The pain occurs after waking up, sitting for a long time, and after exertion.
No distortion at this stage yet. X-ray shows narrowed joint cavity.
How to treat gonarthrosis?
For treatment, a special group of drugs is used - chondroprotectors. They contain chondroitin and glucosamine, which help restore the structure of cartilage and increase elasticity. NSAIDs are used to relieve pain.
Primary gonarthrosis is usually bilateral. Even with the development of one form of the disease, after a while the second limb is also involved in the pathological process.
The initial symptoms of osteoarthritis of the knee are mild and nonspecific
Treatments
In addition to drug treatment in the period of remission, the following methods are used:
- physical therapy;
- Massage;
- leech therapy;
- ultrasonic exposure;
- radon and hydrogen sulfide baths;
- electrophoresis, electrophoresis;
- paraffin coated;
- the use of therapeutic mud.
These methods are used regardless of the stage of disease development during remission.
Is mud good for knee osteoarthritis? One of the indications for mud therapy is diseases of the musculoskeletal system. The course of treatment is carried out twice a year. It consists of 10 to 15 procedures. This method can be used at home, and dirt can be purchased at the pharmacy.
In the first degree, the patient is prescribed to wear orthopedic shoes during the exacerbation period to prevent the development of the deformity process. Women are advised to wear shoes with soles at least 1 cm thick, heels 5 cm. Normalize diet - reduce salt intake, spicy foods. Meats and jellies are included in the diet, as they are natural plant protectors.
Another method is weight correction. Reducing body weight to the optimum level for a given patient will reduce the load on the musculoskeletal system.
Grade 2 gonadal fibroma
In the second degree, the pain is more intense, so movement is significantly limited. Walking for a long time causes severe pain syndrome. The patient needs rest to continue.

If treatment is not started (or doesn't work), the knee osteoarthritis will progress further.
The creaking became loud, and there were limping sounds. The affected joint is deformed. The inflammatory process occurs in the inner membrane of the joint.
On plain X-ray, the joint cavity is narrowed, and bone spurs (osteocytes) appear.
Treatment
Drug therapy is based on the use of NSAIDs. They have analgesic and anti-inflammatory effects. Moreover, chondroprotectors are prescribed.
After the exacerbation passes, physiotherapy exercises, massage are prescribed.
Dietary recommendations:
- increase the amount of vegetables;
- include jelly and meat jelly in the diet;
- eat lean fish twice a week;
- give preference to lean meat;
- eat bran bread.
It is also recommended to include in the diet bananas, nuts, eggs, spinach, legumes, liver, cabbage.
In addition to orthopedic shoes, special knee pads are prescribed.
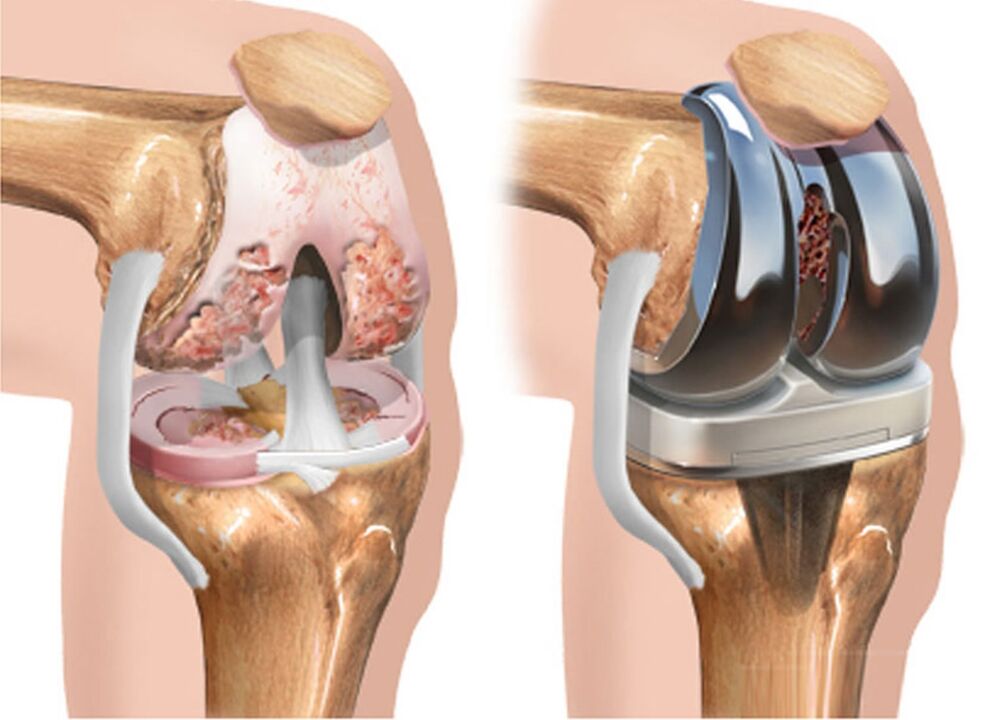
From surgical interventions, arthroscopy to remove deformed tissues is used. This method has a short-term effect of 2 - 3 years.
Knee gonarthrosis, symptoms and treatment grade 3
The heaviest level. Pain syndrome occurs with movement and at rest. The mobility of the knee is as limited as possible, and sometimes not possible. Distortion is pronounced. In fact, there are no common gaps on the positioning chart.
The gradual destruction of cartilage and bone in the final stages leads to the knee developing into ugly deformities, increasing in size.
Treatment
At this stage, in addition to NSAIDs, the patient is prescribed hormonal drugs. They are injected into a vein or inside a joint. Severe pain syndrome relieved by pain medication.
At stage 3, the operation was shown - laparoscopy. Individual bone elements or the entire joint are replaced. Contraindications: osteoporosis.
Complications of arthroplasty:
- marginal skin necrosis;
- refuse prostheses;
- neurovascular disorders (paralysis, thrombosis).
In addition to arthroscopy, there is also a joint operation - removal of deformed tissues and joints. It is rarely used.
Osteotomy - cuts off the edges of the bone to redistribute the load.
Physical therapy
Exercises for the knee joints can relieve pain, strengthen the muscles and stimulate blood flow to them.
- Exercise No. 1. The patient lies on his back, raise his leg straight up and hold it for at least 30 seconds, then perform a second time. The execution time should be taken about 2 minutes.
- Exercise #2 "Bicycle". Lying on your back mimics cycling with your legs. Repeat 20 to 50 times.
- Exercise 3. The patient lies on his stomach, alternately bending his legs, trying to touch his heels to his buttocks. Repeat 20-50 times.
- Exercise #4. It is done in the same way as before, only in static mode. That is, the patient fixed the limb in this position for 20-30 seconds.

Patients are advised to prolong:
- Exercise #1. In a standing position, bend over and try to touch the floor without bending your knees. Hold for 20 seconds, inhale through the nose, exhale through the mouth.
- Exercise #2. Sit on the floor with your legs straight, try to wrap your arms around your feet, while keeping your knees straight. Hold this pose for up to 30 seconds. Take 2-3 approaches. If the leg is not flexible enough, they take the foot with the shin and try to pull the body as close to the leg as possible.
- Exercise #3. Same position as last time. The patient retracts the leg with the foot, tries to straighten it and keep it as high as possible off the floor. If the exercise is difficult to perform, take the foot in the shin area. Hold the pose for 10-30 seconds, then do it with the other leg.
Contraindications are the exacerbation phase and the presence of an acute inflammatory process. The patient is prohibited from running, long walking and squatting.
After performing physical therapy exercises, it is recommended to massage the thigh and lower leg muscles in the painful limb. The joint itself should not be affected, which will increase inflammation.
Disease prevention
The disease is not inherited, so its development can be prevented. This requires:
- avoid injury when playing sports;
- doing stretching and joint exercises, yoga;
- Eat right;
- maintain a normal body weight;
- if you feel discomfort in the knee area, consult your doctor;
- drink enough water;
- after 40 years of age, take prophylactic chondroprotectors;
- do not cool the joints excessively;
- in the initial stages of the process and during remission, do not increase physical activity, do not run;
- wear orthopedic shoes;
- Use knee pads when playing sports.














































